COVID-19 Simulator Informs Local Policymaking: Q&A with Jagpreet Chhatwal, PhD
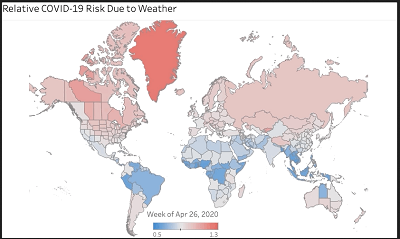
The COVID-19 Simulator , developed by Massachusetts General Hospital, Harvard Medical School, Boston Medical Center and Georgia Tech, was launched in April 2020 to help health policymakers and practitioners make decisions regarding policy and strategy related to the novel coronavirus pandemic. The original tool shows how lifting or continuing physical distancing measures can impact a state’s number of COVID-19 positive tests, hospitalizations and death.
Since launching, the collaborators have expanded on its offerings to help policymakers make decisions at a county level. In this Q&A, Jagpreet Chhatwal, PhD , associate director of the Institute for Technology Assessment at Mass General, describes the new simulation tools available to lawmakers, how the tools can help make opening/closing decisions and his thoughts on the outlook for the upcoming surge of the pandemic.